A 36 year old woman resident of thirumalagiri, farmer by occupation came with cheif complaints of pain in abdomen since 1 month and 1 episode of vomiting associated with blood yesterday
20 April 2023
E LOG GENERAL MEDICINE
Hi, I am Naalla Gayathri , 5th Sem Medical Student.This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent.
Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs.
This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment box is welcome.”
I've been given this case to solve in an attempt to understand the topic of "patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with a diagnosis and treatment plan.
DATE OF ADMISSION: 19th April 2023
CHIEF COMPLAINTS:
Patient complaints of pain abdomen since 1 month and vomiting associated with blood yesterday i.e.on 19th April 2023.
HISTORY OF PRESENT ILLNESS:
Patient was apparently asymptomatic 1 month ago.
Then she developed epigastric pain which is of squeezing type,non radiating.
It could occur after consuming spicy,sour or non veg foods and sometimes relieved after an episode of vomiting. And no positional variation of pain.
She had nearly 10 episodes of vomiting in last month which is non projectile,non bilious type and food as its content.
Yesterday she had 1 episode of hematemesis (blood in vomiting) which is dark brown colour.
No history of fever, bloating, chest pain, retrosternal burning, constipation.
MENSTRUAL AND OBSTETRIC HISTORY:
Menarche : 13 years of age
Marriage: 12 years of age
Cycle: 30/5
3 children( 1st boy ,2nd girl,3rd boy) through cesarean delivery .
PAST HISTORY:
Renal calculi 11 years ago which are excreted in urine by using medication.
And 2 months back again a renal calculi found and relieved by medication.
No history of hypertension,diabetes, asthma, tuberculosis, epilepsy, thyroid.
PRESENT HISTORY:
Diet:mixed
Appetite: normal
Sleep: adequate
Bowel: regular
Bladder: regular
Addictions: Toddy (occassionally) 250 ml
FAMILY HISTORY:
No significant family history
ALLERGIEC HISTORY:
Allergic to fish,brinjal,gongura food items.
1 year she delevoped rash like manifestation on hands.
No history of drug allergy.
GENERAL EXAMINATION:
Patient was conscious, coherent and cooperative.
Well oriented to place,time and person.
Pallor - absent.
No icterus
No cyanosis
No clubbing of fingers
No lymphadenopathy
No edema
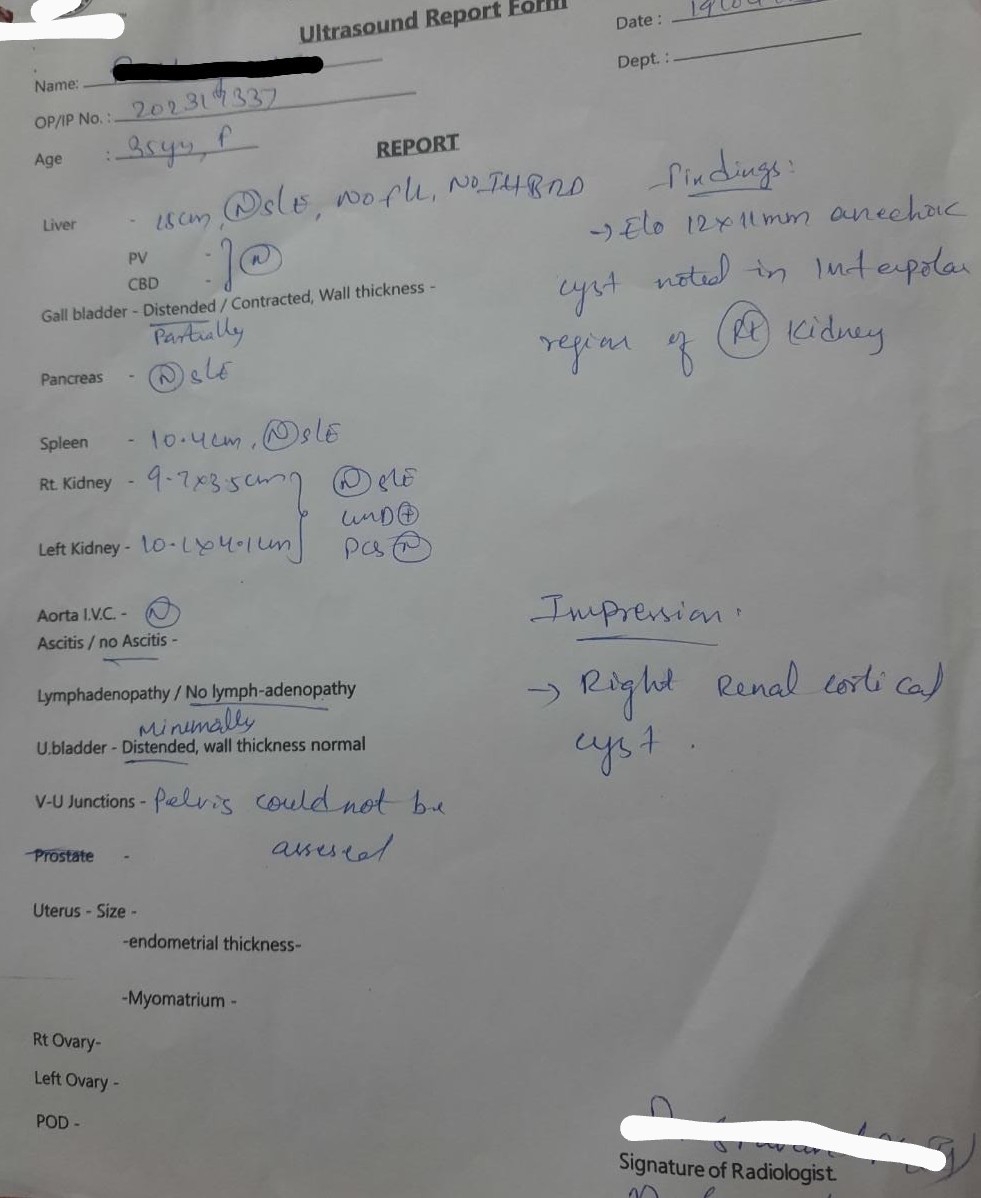
Ultra sound: